Ohio Medicaid MCO Update: Buckeye’s new behavioral health UM policies are paused (Not Effective Jan 1)
Important update for Ohio Medicaid managed care (MCO) behavioral health providers: Buckeye Health Plan has announced a temporary pause on implementing its new behavioral health utilization management policies OH.UM.04, OH.UM.06, OH.UM.07, and OH.UM.09. These Buckeye policy changes will NOT go into effect on January 1, 2026.
Buckeye reports the pause is tied to the Ohio Department of Medicaid (ODM) ARPA reconciliation process (which may take up to ~60 days). Buckeye also notes the policies are expected to remain unchanged and will be implemented as planned once ARPA terms are no longer applicable.
This is a major shake-up for Ohio Medicaid behavioral health billing and documentation workflows—especially for IOP, TBS/PSR, and Peer Support—and we’re seeing confusion in the field. Below is a clear breakdown of what’s paused, what was expected to change, and what you should do now.
Buckeye Health Plan (Ohio Medicaid MCO): What’s paused + what still applies
Buckeye has paused implementation of the following new behavioral health policies: OH.UM.04, OH.UM.06, OH.UM.07, OH.UM.09.
Key note: Buckeye indicates that, during the pause, these services will continue to be subject to retrospective utilization review to support medical necessity oversight.
Buckeye also states it plans to host provider webinars in mid-January to review PA thresholds, submissions, appeals/denials, documentation, and portal tracking.
Molina Healthcare — IOP Documentation Expectations (billing + compliance)
Molina’s published reimbursement policy for IOP group counseling (H0015HK) includes documentation expectations tied to billed units:
- Providers billing ≤ 14 units (days) per member per 30 days (month): clinical records not required for compliance verification
- Providers billing > 14 units (days) per member per 30 days (month): clinical records required to verify compliance
Molina also notes compliance verification may include provider qualification guidance and time-based requirements, including at least 2 hours and 1 minute of treatment per unit.
Molina full policy link:
https://www.molinahealthcare.com/-/media/Molina/PublicWebsite/PDF/Providers/common/PIA-Payment-Policies/Molina-PI-Policy-Website/2025-Policies/Intensive-Outpatient-Treatment-Services.ashx
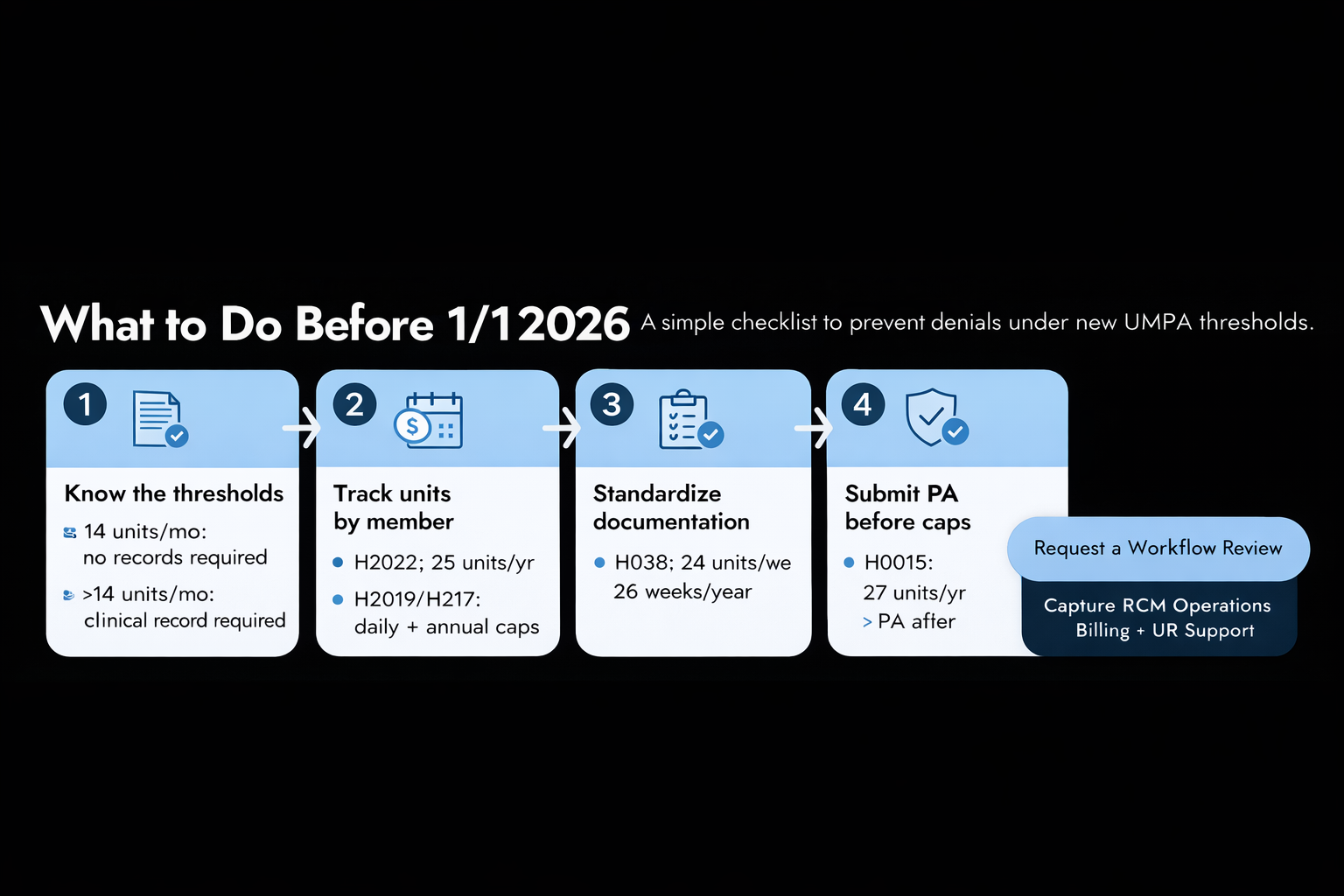
Buckeye (Paused) — Behavioral Health UM/PA Threshold (Once Implemented)
Even though implementation is paused, the thresholds below reflect what Buckeye has published for Ohio Medicaid behavioral health services.
TBS & PSR (OH.UM.04)
- H2020: 25 units/year → PA required after
- H2019: 8 units/day, 80 units/year
- H2017: 8 units/day, 120 units/year
Buckeye policy PDF (OH.UM.04):
https://www.buckeyehealthplan.com/content/dam/centene/Buckeye/policies/clinical-policies-for-updates-starting-10-30/OH.UM.04%20Ohio%20TBS%20and%20PSR%20Policy%20from%20Stacy%2011-12_R.pdf
Peer Support (OH.UM.07)
- H0038: 24 units/week for 26 weeks/year
Buckeye policy PDF (OH.UM.07):
https://www.buckeyehealthplan.com/content/dam/centene/Buckeye/policies/clinical-policies-for-updates-starting-10-30/OH.UM.07%20Ohio%20Peer%20Support%20Services%20from%20Stacy%2011-12_R.pdf
Intensive Outpatient Program (IOP) (OH.UM.09)
- H0015: 27 units/year → PA required after
Buckeye policy PDF (OH.UM.09):
https://www.buckeyehealthplan.com/content/dam/centene/Buckeye/policies/clinical-policies-for-updates-starting-10-30/OH.UM.09%20Ohio%20Intensive%20Outpt%20Policy%20from%20Stacy%2011-12_R.pdf
Buckeye summary page:
https://www.buckeyehealthplan.com/providers/updates11/PAandPolicyUpdates.html
Multiple Services on the Same Date of Service (OH.UM.06)
This is one of the policies Buckeye included in the pause notice. Once implemented, Buckeye’s published summary includes limits such as:
- H0036, H2019, H2017: limited to 16 combined units/day
- If billed on the same date as per diem codes H0015, H2020, or H0015TG, then H0036/H2019/H2017 are limited to 4 combined units/day
Buckeye summary page: https://www.buckeyehealthplan.com/providers/updates11/PAandPolicyUpdates.html
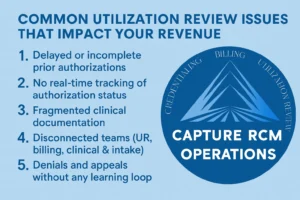
Recommendations for Providers & Billing Teams
(During the Buckeye Pause)
Because Buckeye has paused implementation (and the effective date is now TBD), the goal right now is to reduce confusion, protect documentation quality, and get workflows ready for when Buckeye turns these on.
- Communicate the pause internally (clinical + UR + billing) so teams aren’t preparing for a Jan 1 go-live that isn’t happening.
- Review the published Buckeye policies (OH.UM.04 / 06 / 07 / 09) and map which services you bill that hit these thresholds.
- Train teams on documentation fundamentals that withstand retrospective UR (medical necessity, time, qualified provider, treatment-plan linkage). Buckeye explicitly notes services remain subject to retrospective review during the pause.
- Update templates + tracking so you can:
- Track units by member (weekly/monthly/yearly caps)
- Flag threshold approach early
- Standardize clinical summaries to match time/unit expectations (especially IOP)
- Standardize clinical summaries to match time/unit expectations (especially IOP)Prepare PA workflows in advance so you’re not scrambling when Buckeye re-activates implementation.