When you’ve handled billing in-house for years, switching to a vendor feels personal. Especially if your team includes people who’ve walked the recovery path themselves. But utilization review isn’t just about paperwork. It’s about understanding the story behind the treatment—and making sure it’s heard, documented, and reimbursed.
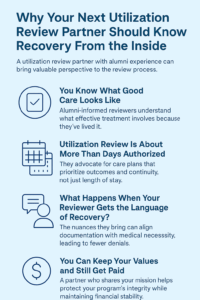
You Know What Good Care Looks Like—But Does Your RCM Partner?
If you’ve been through treatment yourself, you know what real care feels like. You also know when a provider is just checking boxes. The same is true in utilization review. A good RCM partner doesn’t just recite DSM codes. They advocate for the clinical picture as if it’s their own—because sometimes, it is.
Why Alumni-Informed Review Matters
A reviewer who understands relapse patterns, trauma responses, or why a client might stall in week three of PHP doesn’t just submit a stronger case. They tell a story insurance can recognize. That kind of nuance comes from experience, not just credentials.
Utilization Review Is About More Than Days Authorized
You’re not just fighting for bed days. You’re fighting for continuity, for outcomes, and for care plans that don’t get cut short. A utilization review and compliance team trained in both documentation and real-world treatment dynamics makes a tangible difference in how consistently you get reimbursed—and how many times you have to fight the same battle.
What Happens When Your Reviewer Gets the Language of Recovery?
We’ve seen the difference it makes when reviewers speak the same language as your clinical team. They don’t miss red flags. They anticipate pushback. And they know how to translate behavioral progress in a way that aligns with medical necessity criteria. That alignment means fewer denials, fewer peer-to-peers, and more time for your staff to focus on what matters: treatment.
A Change That Respects Your Team’s Legacy
Outsourcing RCM doesn’t mean erasing your history. It means finding a partner who honors it. One who recognizes how hard your team has worked to build trust, retain staff, and keep care relational. Capture RCM isn’t just another vendor—they’re a clinical-aligned partner who brings operational clarity to emotionally driven work.
You Can Keep Your Values and Still Get Paid
Switching utilization review providers isn’t just a business decision—it’s a cultural one. Choose a team that understands how your alumni think, how your clinicians speak, and why your program is different. That’s how you protect your mission while making the financial side sustainable.
Ready to work with a team that sees the whole picture?
Call (380) 383-6822 or visit to learn more about our utilization review services in United States.