Starting a treatment center means making a thousand decisions a week—and utilization review probably wasn’t at the top of your list. But if you want to get paid by insurance, stay compliant, and avoid financial fire drills, it should be. At Capture RCM Operations, we help new programs set up strong utilization review processes before their first client even walks through the door.
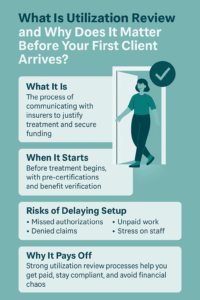
What Is Utilization Review?
Utilization review (UR) is the structured process of justifying medical necessity to insurance companies. It’s how treatment centers prove that a client actually needs the level of care they’re receiving—and that it should be reimbursed.
In simple terms? It’s how you keep treatment authorized and funded.
Why Utilization Review Starts Before Treatment Does
Most founders assume UR is something you handle after a client is admitted. But in reality, it begins with pre-certifications, verification of benefits, and documenting eligibility before care even starts. Without that structure in place early, your clinical team can end up doing urgent backtracking while your billing stalls.
The Hidden Cost of Delaying UR Setup
If you’re scrambling to get UR systems in place mid-treatment, you risk:
- Missed or delayed authorizations
- Denied claims
- Unpaid services
- Strained staff communication
- And potentially noncompliance
That’s not just paperwork stress—it’s revenue left on the table.
Who Handles Utilization Review—and Why It Can’t Be Just Anyone
UR isn’t just data entry. It requires clinical insight, payer knowledge, and strong documentation. Many new programs make the mistake of assigning it to someone without training—or asking a busy clinician to double up. A professional utilization review team, like ours at Capture RCM Operations, protects both your revenue and your clinical credibility.
What a Good Utilization Review Partner Provides
A strong UR partner gives you:
- Payer-specific documentation guidance
- Real-time authorization tracking
- Scheduled reviews and reminders
- Direct insurer communication
- And clear handoffs to billing teams
Most importantly, they create a rhythm—so your team isn’t reacting, they’re running things with confidence.
Compliance and Credentialing: The Overlooked Foundations
Before utilization review can even happen, your program has to be set up to legally deliver and bill for care. That means your clinicians must be properly credentialed with payers, and your documentation must meet basic compliance standards. Without these two pieces, even the best UR strategy will hit roadblocks.
Credentialing ensures your providers are recognized by insurance panels, while compliance keeps your charts audit-ready. When these are missing or incomplete, insurers can delay or deny reimbursement—no matter how medically necessary the care was.
A good RCM partner doesn’t just chase authorizations. They help make sure your foundation is solid—so UR, billing, and reimbursement all flow smoothly from the start.
Build Before the Rush
Getting your utilization review systems in place early means fewer surprises later. It means your clinicians can focus on care, your billing team can work efficiently, and your leadership can breathe.
Want Support from Day One?
Call (380) 383-6822 or visit to learn more about our utilization review services in United States. We’ll help you set up systems that make your first year smoother—and more sustainable.