Prevent Treatment Disruptions with Utilization Review Support
When someone is newly diagnosed, they need steadiness: clear next steps, consistent care, and fewer surprises. But when a program is growing fast, that steadiness can get threatened by paperwork bottlenecks—especially around authorizations and continued-stay reviews.
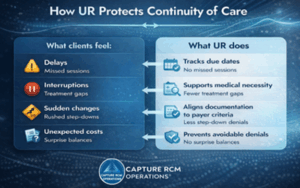
That’s where utilization review support can quietly keep the whole plan standing. Done well, utilization review protects the treatment plan so clients don’t feel the administrative turbulence behind the scenes.
What Utilization Review Is (And What It Isn’t)
Utilization review (UR) is the clinical-and-payer “translation layer” that shows medical necessity, level of care, and continued need—so treatment can be authorized and reimbursed appropriately. Capture RCM describes UR as ensuring care is medically necessary, appropriate, and aligned with payer requirements while reducing denials and delays.
What it isn’t: a cold gatekeeping function that fights your clinicians. Done well, utilization review protects clinical judgment by documenting it in a way payers recognize.
Memorable truth: UR is the handrail on the stairs, and patients may not notice it, but it prevents a fall.
Why Utilization Review Matters Most For Newly Diagnosed Clients
Newly diagnosed clients often arrive with a mix of fear and hope. They’re asking, sometimes without words: “Is this real? Will you help me? Am I going to get dropped?”
When authorizations stall or continued stays aren’t approved in time, clients experience it as instability:
- Missed sessions
- Rushed step-downs
- Treatment interruptions
- Unexpected bills or “surprise” balances
UR helps prevent those breaks by keeping approvals current and aligned to payer expectations throughout treatment—not just at intake.
UR And Denials: How To Avoid The Most Common Breakdowns
Most denials aren’t personal—and they’re often preventable. The patterns usually come down to timing, alignment, or clarity:
1) Timing issues
- authorization requests submitted late
- continued-stay reviews missed
- step-downs not supported early enough
Fix: work off a predictable review calendar, with clear due dates and escalation rules.
2) Alignment gaps
Documentation doesn’t clearly connect:
symptoms → impairment → level of care → plan → progress → continued need
Fix: require a “throughline” in notes that ties clinical reality to payer criteria.
3) Clarity problems
- vague notes
- missing criteria language
- inconsistencies across records (assessment vs. progress note vs. treatment plan)
Fix: standardize templates and do quick clinical QA before submission.
Capture RCM’s UR approach includes authorization management, clinical review for medical necessity, and ongoing compliance monitoring, exactly the areas that reduce “avoidable denials.”
Insert Alt text: Utilization review in behavioral health infographic showing how UR protects continuity of care by preventing treatment delays, interruptions, rushed step-downs, and surprise bills.
When You Want To Take More Clients, But Credentialing Delays Make You Hesitate
This is a real CEO moment: your phone is ringing, referrals are strong, and your clinicians are ready, but credentialing timelines and payer enrollment lag behind your growth.
That stress makes sense. Credentialing is a known revenue bottleneck in behavioral health, and if it’s off by even a little, claims and authorizations can unravel.
If you’re feeling the tension between serving more people and protecting reimbursement, consider pairing credentialing support and utilization review support.
That combination helps you grow without forcing your clinical team to carry the administrative weight.
A UR Workflow A CEO Can Oversee Without Drowning In It
You don’t need to micromanage UR to lead it well. You need visibility and a clean rhythm.
A practical oversight structure looks like this:
- One weekly snapshot: Pending auths, due dates, recent denials, and appeals in motion
- Clear ownership: Who submits, who documents, who follows up, and who escalates
- A “no surprises” rule: If a continued stay is at risk, you hear about it early—before the client feels it
Capture RCM positions UR as a way to streamline authorizations and prevent unnecessary delays while safeguarding the revenue cycle.
What To Look For When Outsourcing Utilization Review And Compliance
Outsourcing should create calm and not confusion. Look for a partner who can:
- Speak both languages: clinical logic and payer requirements
- Track shifting rules and keep you audit-ready (not reactive)
- Coordinate with credentialing, billing, and compliance as one system (not separate silos)
You’re not “behind.” You’re building, while people are counting on you. If you want to take more clients with confidence (without letting UR, credentialing, or compliance gaps create preventable denials), get expert support.
Quick FAQ
How often are authorizations reviewed?
It depends on payer and level of care. Many require continued-stay reviews on a set cadence (e.g., every few days early on, then weekly).
What documentation is most likely to trigger denials?
Notes that don’t show functional impairment, don’t support the level of care, or don’t demonstrate ongoing need/progress.
Can outsourcing UR reduce clinician burnout?
Yes, when the outsourced team owns timelines, payer communication, and submission quality control, clinicians spend less time chasing paperwork.