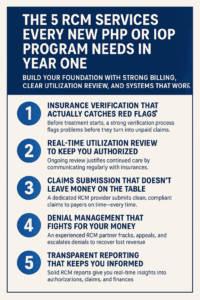
Starting a PHP or IOP program is bold—and sometimes brutally overwhelming. Between compliance requirements, clinical staffing, and getting your first clients in the door, it’s easy to overlook revenue cycle management. But skipping this step early can cost you big later. Services like utilization review aren’t just “nice to have”—they’re essential to keeping your program funded and running.
1. Insurance Verification That Actually Catches Red Flags
Before you treat a client, you need to know what their plan covers—and what it doesn’t. This isn’t just about checking boxes. A strong verification process catches things like plan carve-outs, mental health limits, and out-of-network risk. RCM teams dig into the fine print and flag problems before they turn into unpaid claims.
2. Real-Time Utilization Review to Keep You Authorized
Utilization review is where a lot of new programs struggle. It’s the ongoing communication between your team and insurance providers that justifies continued care. If it’s late, incomplete, or missed? You won’t get paid. Outsourcing this to a company like Capture RCM Operations gives your clinical team room to focus on care—not documentation deadlines.
3. Claims Submission That Doesn’t Leave Money on the Table
You’d be shocked how often small mistakes delay thousands in revenue. Missing modifiers, incorrect taxonomy codes, or simply using the wrong payer portal can all trigger denials. A dedicated RCM partner ensures your claims are clean, compliant, and submitted on time—every time.
4. Denial Management That Fights for Your Money
Insurance companies don’t always play fair. Even strong claims in a PHP or IOP get denied. Without a process to track, appeal, and escalate, revenue leaks fast. An experienced RCM provider will flag trends, rework denials, and recover lost funds—so you’re not constantly playing catch-up or leaving revenue uncollected.
5. Transparent Reporting That Keeps You Informed
In your first year, clarity is everything. A solid RCM company should give you real-time reports on authorizations, claims status, aging reports, and financial forecasts. This data helps you grow wisely and make decisions based on facts—not feelings or fire drills.
You Don’t Have to Do This Alone
Trying to run clinical operations and manage the financial back end is a recipe for burnout. These five RCM services—especially utilization review—create the operational breathing room you need to focus on care, community, and quality.
Let’s Make Your First Year Strong
Call (380) 383-6822 or visit to learn more about our utilization review services in United States. We’ll help you get paid, stay compliant, and build a program that lasts.