For small behavioral health practices, staying compliant with payer requirements isn’t just a regulatory necessity—it’s a direct factor in whether you get paid, how quickly, and how consistently. Unfortunately, one of the most overlooked drivers of billing compliance and revenue risk is utilization review (UR).
Many practice owners try to manage utilization review internally—assigning the task to an office manager or asking clinicians to handle it alongside client care. But UR isn’t just a formality. It’s a technical, time-sensitive process that requires expertise in payer criteria, documentation alignment, and ongoing communication with insurance reviewers.
In this guide, we’ll explore the business case for professional utilization review services, including how UR impacts your revenue cycle, what compliance risks to watch for, and how to decide whether to handle it in-house or outsource to a partner like Capture RCM Operations.
What Is Utilization Review and Why Does It Matter?
Utilization review (UR) is the structured evaluation of whether a patient’s behavioral health services are medically necessary, appropriate, and aligned with payer coverage criteria. It typically includes:
- Initial authorization requests (before services begin)
- Concurrent or continued stay reviews (mid-treatment)
- Step-down reviews (when transitioning levels of care)
- Appeals of denied services
For services like PHP, IOP, and residential treatment, utilization review is required to obtain and maintain authorization from insurance carriers. Without approved UR, even the best-delivered care may go unpaid.
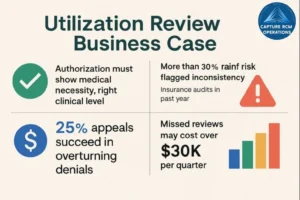
What small practice owners often don’t realize is that poor UR management affects far more than reimbursement. It can trigger compliance flags during payer audits, lead to recoupments, and reduce approval rates for future clients.
The Hidden Risks of In-House UR Management in Small Practices
Most small practices handle UR internally out of necessity, but this approach carries several hidden risks—especially when staff are stretched thin or lack payer-specific training.
1. Missed Authorization Windows
Each payer has specific timeframes for submitting continued stay reviews. Miss one by even a day, and you may lose reimbursement for multiple sessions or entire treatment blocks.
2. Insufficient Documentation of Medical Necessity
Payers expect UR submissions to reflect clinical acuity using specific language tied to their criteria. Generic or vague notes—even if clinically valid—can lead to denials.
3. Overburdened Clinical Staff
When therapists are responsible for both delivering care and managing UR communication, something suffers—either quality time with clients or accuracy in submissions.
4. No Appeals Infrastructure
Many small practices don’t have a system for tracking and appealing denied reviews. Denied sessions often go unchallenged, resulting in preventable write-offs.
Case Example:
A small IOP practice in Pennsylvania lost over $30,000 in one quarter after missing multiple concurrent review windows. Without dedicated UR staff or a denial log, leadership didn’t realize how much revenue had slipped through until their CPA flagged unexplained variances.
How Utilization Review Services Support Compliance and Revenue
Professional utilization review services don’t just reduce administrative workload—they create operational guardrails that protect your practice from denials, lost revenue, and audit risk. Here’s how:
Streamlined Review Submissions
A dedicated UR team ensures that all initial and continued stay reviews are submitted on time, with payer-specific formatting and required documentation.
Enhanced Documentation Quality
Reviewers are trained to translate clinical progress into the language payers require. They coach providers or use structured templates to ensure medical necessity is clearly supported.
Centralized Payer Communication
UR services manage back-and-forth communication with insurance reviewers, respond to requests for additional information, and escalate issues before they become billing problems.
Denial Tracking and Appeals
When reviews are denied, the UR team logs them, drafts appeals, and works with clinical leadership to correct the issue—turning potential write-offs into reimbursed sessions.
Aligned Clinical and Billing Workflows
Professional UR teams work closely with billing and credentialing staff to ensure there’s alignment on CPT codes, level-of-care authorizations, and policy changes.
A Business Framework to Evaluate “Build vs. Buy”
If you’re trying to decide whether to manage UR in-house or outsource, use this decision framework:
| Business Factor | In-House UR | Outsourced UR Services |
|---|---|---|
| Cost Structure | Fixed (salaries, admin time) | Flexible (per-review or flat monthly) |
| Staff Capacity | Often overloaded | Frees up internal staff |
| Compliance Risk | Higher if undertrained | Lower due to expertise |
| Scalability | Limited by FTEs | Easily scales with client volume |
| Payer Knowledge | General | Deep, specialized |
| Denial Management | Inconsistent | Systematic tracking and appeals |
| Audit Preparedness | Reactive | Proactive and documented |
If your practice has more than 10–15 clients requiring high-acuity care at any given time, it may be more cost-effective—and safer from a compliance perspective—to outsource.
Audit Your Current UR Process With This Checklist
Before deciding on an outsourcing partner, assess your current capabilities.
Utilization Review Audit Checklist:
- Do we submit initial and continued stay reviews on time for every client?
- Do we have payer-specific templates for UR documentation?
- Who manages communication with insurance reviewers?
- How often are reviews denied? Are reasons tracked and analyzed?
- Do we have a process for submitting appeals?
- How is feedback from denials communicated to clinicians?
- Are missed or delayed UR submissions causing lost revenue?
If you answered “no” or “unsure” to more than two of these questions, your practice could benefit from structured UR support.
Align Clinical Staff With UR Compliance Expectations
Even with external UR support, clinical documentation remains the foundation of every review. Small practice owners can improve outcomes by aligning their team around these practices:
Provide UR Training for Clinicians
Ensure providers understand how medical necessity is evaluated and how their notes support authorization decisions.
Use Structured Progress Note Templates
Templates help ensure key details—risk levels, functional impairments, and treatment response—are consistently documented.
Establish Internal Deadlines
Build calendar reminders and checklists into your EHR workflow to avoid last-minute UR submissions that may miss critical payer windows.
Share Denial Trends With the Team
Turn denials into learning opportunities by debriefing clinicians on what language or documentation gaps led to rejection.
When to Transition to Professional UR Services
Outsourcing isn’t just for large practices. It’s a strategic move for small teams looking to grow without increasing administrative complexity. Consider outsourcing when:
- You’re seeing higher denial rates without clear trends.
- Clinical staff are burning out under documentation and admin demands.
- You’ve lost revenue due to missed reauth or delayed UR submissions.
- You’re expanding to higher levels of care (e.g., adding PHP or IOP).
- Audits or payer reviews have flagged inconsistencies in your UR process.
Capture RCM’s Utilization Review Services are designed for behavioral health organizations that need expertise without adding headcount. Our team ensures compliance, reduces billing risk, and helps your practice scale with confidence.
Frequently Asked Questions
What exactly does a utilization review team do?
They manage the submission of initial and continued stay reviews to payers, align clinical documentation with medical necessity criteria, communicate with insurance reviewers, and appeal denials as needed. They serve as the compliance layer between clinical care and billing.
How can I tell if our current UR process is putting us at risk?
Look for patterns such as increased denials, staff complaints about admin burden, missed deadlines for reviews, or unexplained revenue shortfalls. If you’re not tracking UR metrics, that’s a red flag in itself.
Is UR only necessary for higher levels of care like PHP and IOP?
Most commonly, yes. However, some insurers now require UR even for outpatient services after a set number of sessions. Knowing payer-specific requirements is part of staying compliant.
Won’t outsourcing cost more than managing it ourselves?
Not necessarily. When you factor in staff time, denied claims, and lost revenue from missed deadlines, outsourcing can save money while improving outcomes. Many services offer per-review pricing that scales with your needs.
What happens if a review is denied?
A professional UR team will identify the denial reason, coordinate with clinicians to strengthen documentation, and submit an appeal. They track these outcomes and adjust future submissions to prevent repeat issues.
Take the Complexity Out of Utilization Review
Compliance isn’t just about following rules—it’s about protecting the business you’ve built. Utilization review is one of the most critical links between your clinical services and your ability to get paid. Done right, it boosts revenue, improves payer relationships, and reduces stress across your team.
Call (380) 383-6822 or visit Capture RCM’s Utilization Review Services to learn how we support small behavioral health practices with expert-level UR systems that strengthen compliance and support sustainable growth.