When you’re ready to grow your behavioral health program—but keep running into credentialing bottlenecks—it’s more than frustrating. It can feel like your capacity to help people is stuck in someone else’s inbox. Outsourcing utilization review might be the quiet shift that changes everything.
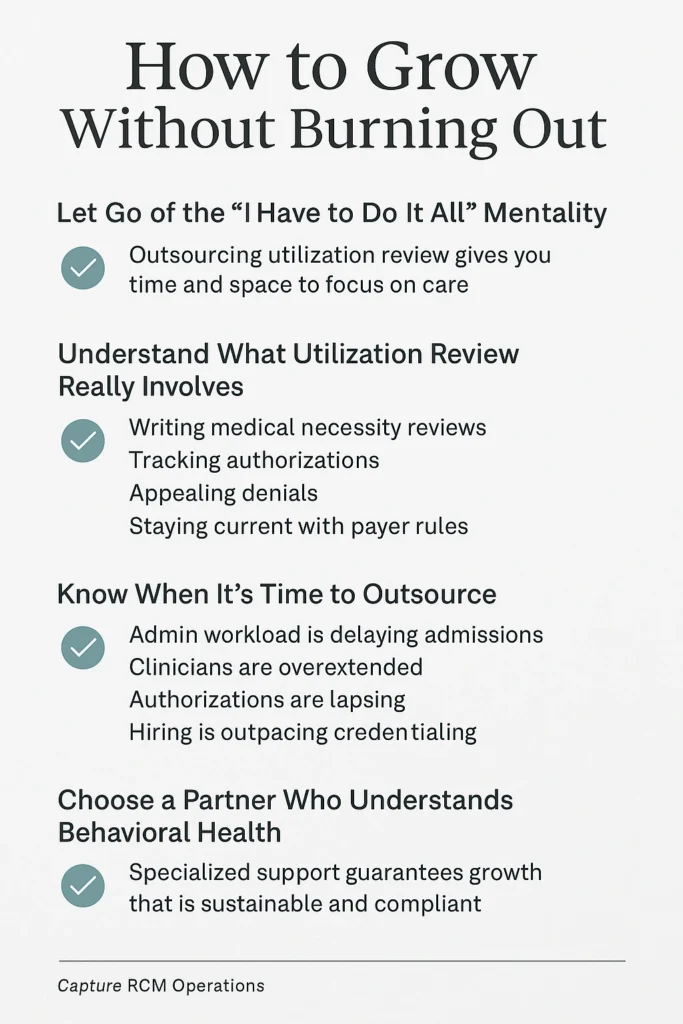
Let Go of the “I Have to Do It All” Mentality
As a clinician-turned-CEO, your role has evolved—but your heart’s still in the clinical work. And yet, utilization review, compliance logs, and payer policies have become part of your daily life. That kind of mental load creates tension: your mission grows, but so does the paperwork.
Outsourcing UR doesn’t mean giving up control. It means choosing support so you can focus on care, not codes.
Understand What Utilization Review Really Involves
At its core, utilization review (UR) ensures that your clients’ care is covered—and justified—in the eyes of insurance. But that includes:
- Writing medical necessity reviews
- Tracking authorizations across levels of care
- Appealing denials with precise documentation
- Staying current with evolving payer rules
If your team is already stretched, UR tasks can quietly delay admissions or lead to lapses in care continuity.
Know When It’s Time to Outsource
Some signs that it’s time to get help with utilization review:
- You’re turning away clients due to capacity—not in the clinic, but in your admin workflow.
- Your clinicians are writing reviews at night, feeling burned out.
- Authorizations are expiring because no one had time to track them.
- You’re hiring—but credentialing and compliance are lagging behind.
One CEO told us, “We had the clinical team ready. We just couldn’t keep up with the backend approvals.” You’re not alone in this.
What Outsourcing UR Can Actually Do for You
With the right support team, outsourced utilization review becomes an engine for growth. At Capture RCM Operations, our UR services:
- Submit timely, payer-specific medical necessity reviews
- Track and renew authorizations proactively
- Document care transitions clearly and cleanly
- Manage appeals with experience, not guesswork
- Provide full transparency so you always know what’s pending
Most importantly, we free up your staff to do what only they can—provide excellent care.
Stay Compliant Without the Constant Scramble
UR and compliance don’t just affect revenue—they protect your program’s credibility. When you outsource to a team that specializes in behavioral health, you’re not just covering the basics. You’re ensuring that:
- Each chart supports medical necessity
- Transitions in care are documented and billed properly
- Denials don’t quietly cost you thousands
- Your audits are clean, your clinicians are supported, and your growth is sustainable
Choose a Partner Who Understands Behavioral Health
You don’t need a generic billing company. You need a partner who understands what it’s like to run an IOP, onboard new clinicians, and navigate prior authorizations for teens in crisis. Our utilization review services were built for programs like yours—where every client matters, and every approval counts.
📞 Call (380) 383-6822 or visit to learn more about our utilization review services in United States.