In behavioral health billing, denials are more than just annoying—they’re expensive. And while many billing managers are skilled at correcting coding issues or chasing down missing information, one category of denial continues to drain revenue with frustrating regularity: services denied for authorization or medical necessity reasons.
These denials are often avoidable. But only if they’re caught before the claim is submitted—when utilization review (UR) happens.
If you’re drowning in claim rework, retroactive authorizations, or appeals tied to documentation gaps, it’s time to rethink your workflow. This is where utilization review services step in. Not as a bolt-on to billing—but as a foundational process that makes billing clean, compliant, and far more predictable.
The Denial Patterns Every Billing Manager Should Be Tracking
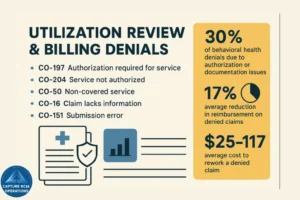
Denials related to authorization or documentation aren’t random—they’re systemic. Billing managers should recognize and log these common denial codes and rationales:
- CO-197: Authorization required for service
- CO-204: Service not authorized
- CO-50: Non-covered services (often tied to lack of medical necessity)
- CO-16: Claim lacks information (often missing authorization or review)
- CO-151: Payment adjusted due to provider submission error
Most of these issues don’t begin with a billing mistake—they begin with missing or delayed utilization review. And without a structured UR process in place, these denials will continue to appear, even if your billing execution is flawless.
What a Broken UR Process Looks Like in Billing Operations
If your billing team is constantly following up on missing authorizations or appealing denials tied to medical necessity, your upstream processes are broken. Here’s what that often looks like:
- No formal tracking system for initial or continued stay reviews
- Authorizations expiring mid-treatment without alerts
- Billing submitted before authorization is confirmed
- Denials discovered only during remittance review
- Clinical teams unaware of payer-specific documentation expectations
- Appeals handled without supporting clinical justification
Sound familiar? You’re not alone. In small and mid-sized behavioral health practices, the lines between billing, clinical, and administrative duties are often blurry. But when UR is not formalized—or worse, delegated inconsistently—the result is a billing process that’s always reactive and often revenue-negative.
How Utilization Review Services Solve the Root Problem
A professional utilization review service steps in before billing begins, solving the foundational issues that create preventable denials.
Here’s how UR services directly improve billing outcomes:
1. Pre-Authorization Management
Every new admission or level of care transition requires authorization. UR services submit these requests with the correct documentation, ensuring approvals are in place before services begin.
2. Continued Stay Review Timelines
Most payers require ongoing reauthorization every 5–7 days for PHP or IOP. UR services maintain calendars, submit reviews on time, and avoid service gaps that billing cannot recover.
3. Documentation Review for Medical Necessity
Before submitting to payers, UR teams review clinical notes to ensure they support the level of care, using ASAM or payer-specific criteria. This prevents downstream denials tied to “non-covered” services.
4. Payer Communication
UR services interface directly with payer reviewers—handling questions, submitting addendums, and resolving issues in real time, so billing doesn’t inherit incomplete cases.
5. Appeals and Denial Tracking
When a denial does occur, UR teams lead the appeal process—drafting clinically sound justifications that billing teams may not be equipped to write.
The result: fewer denials, faster payments, and a more stable revenue cycle.
Aligning UR and Billing: A Practical Integration Model
Even with outsourced UR services, billing managers must ensure operational integration. Here’s a model that connects both teams for seamless claim execution:
| Stage | UR Responsibility | Billing Responsibility |
|---|---|---|
| Pre-Service | Submit authorization with clinical documentation | Verify approved CPTs and units before scheduling |
| Mid-Treatment | Submit continued stay review with updated notes | Monitor authorization expiration alerts |
| Post-Treatment | Log approval or denial outcome | Match billed services to authorized services |
| Claim Submission | Alert billing to denied or pending services | Only bill approved services with valid auth |
| Denial Follow-Up | Draft and submit appeals with clinical rationale | Track response and post-payment adjustments |
This shared process keeps both functions in sync—preventing billing from reacting to surprises that should have been addressed earlier in the cycle.
Financial Impact of Authorization-Related Denials
Let’s look at the numbers.
According to industry benchmarks:
- The average cost to rework a denied claim is $25–$117 per claim
- Denied claims reduce reimbursement by an average of 17%
- In behavioral health, up to 30% of denials are tied to authorization or documentation issues
For a 20-client PHP program billing $1,200 per client weekly, a single missed continued stay review could mean $4,800–$6,000 in unreimbursed care. Multiply that across a quarter or a year, and you’re looking at tens of thousands in preventable losses.
UR services don’t just “help” billing—they prevent revenue leaks you might not even be fully measuring.
When to Transition From Manual to Professional UR
Billing managers often inherit poorly defined UR processes—manual spreadsheets, clinician-submitted reviews, or “someone handles it” systems. That’s manageable for small caseloads. But growth reveals the cracks.
Here are signs it’s time to upgrade:
- Denials for “no auth” or “expired auth” appear weekly
- Your billing staff is writing or reviewing appeals
- No system exists for tracking authorization windows
- You’re losing more than 3–5% of projected revenue to preventable denials
- Appeals are delayed because you’re waiting on documentation corrections
Capture RCM’s Utilization Review Services eliminate these issues by providing:
- Dedicated UR coordinators
- Payer-specific documentation support
- Automated reauth tracking and submission
- Appeal and audit preparation
- Full integration with billing workflows
Key Metrics to Track Before and After UR Service Adoption
To quantify the ROI of utilization review, track these KPIs before and after implementation:
| Metric | Pre-UR Service | Post-UR Service |
|---|---|---|
| Denials for “no auth” | High | Reduced by 70–90% |
| Denials for “not medically necessary” | Frequent | Drops as documentation improves |
| Average appeal turnaround | 10+ days | 2–3 days |
| Reimbursement time | Delayed | Improved |
| Staff time spent on rework | Excessive | Significantly reduced |
Frequently Asked Questions
Do utilization review services replace the billing team?
No. UR services work alongside billing—not instead of it. They ensure the services billed were properly authorized and documented, so billing can proceed without delays or denials.
What happens when a payer denies an authorization?
UR teams handle the appeal process. They review the clinical documentation, identify any gaps, and submit a payer-specific appeal with supporting notes and rationale—freeing billing staff from having to manage this process.
Will our clinicians need to change how they document?
Possibly—but in a good way. UR teams provide guidance and templates that help clinicians align notes with payer expectations, especially for higher levels of care like PHP or IOP.
Is there a compliance benefit beyond fewer denials?
Yes. Structured UR processes reduce audit risk by creating a defensible documentation trail. If a payer performs a retrospective review, you’ll have clean records of authorization timing, criteria used, and clinical justification.
How long does it take to implement UR services?
Capture RCM typically onboards UR clients in 1–2 weeks, depending on practice size and payer mix. The setup includes review schedules, system access, and clinical alignment sessions.
The Bottom Line for Billing Managers
If you’re tired of chasing missing authorizations, appealing vague medical necessity denials, or reconciling preventable write-offs, it’s time to stop fighting fires—and start fixing the system that’s causing them.
Call (380) 383-6822 or visit Capture RCM’s Utilization Review Services to streamline upstream compliance, reduce billing denials, and finally create a claims process you can trust from start to finish.