You’ve got your license. Your team is ready. Your first clients are calling.
And now… the insurance panels.
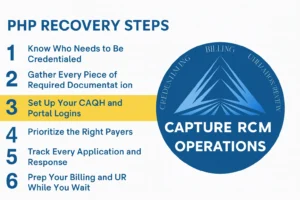
If you’re feeling overwhelmed, you’re not alone. Credentialing is one of the most frustrating early steps for new behavioral health practices—but it doesn’t have to derail your momentum. Capture RCM’s credentialing services help programs like yours get paneled cleanly, quickly, and without the email ping-pong. But if you’re doing it solo for now, this checklist will guide you through the key steps.
1. Know Who Needs to Be Credentialed
Start with your roster.
Credentialing varies by license type, role, and service. Don’t assume everyone needs the same process. Some payers also require facility credentialing—especially for group practices offering PHP, IOP, or wraparound services.
Take the time upfront to clarify who needs what. It will save you months of back-and-forth later.
2. Gather Every Piece of Required Documentation
This is where 80% of delays happen.
Make sure you’ve collected and reviewed these items for each provider:
- National Provider Identifier (NPI) numbers (individual and group)
- State licenses (must be active and up to date)
- Malpractice insurance details
- CVs or resumes
- Tax ID and W-9
- CAQH profiles that are current and attested
Credentialing is a paperwork puzzle—one missing piece can freeze the whole picture.
3. Set Up Your CAQH and Portal Logins
Don’t let portal pain slow you down.
Many payers use CAQH, but others (like Medicaid or smaller commercial plans) have their own systems. Keep a shared folder with login credentials and portal info for each provider. Having this ready saves weeks of rework when it’s time to follow up.
4. Prioritize the Right Payers
Start with who your clients actually use.
You don’t need to be on every panel. Choose 3–5 payers based on your region, population, and referral relationships. Consider Medicaid and any local EAPs. If a panel is closed, don’t panic—ask about gap exceptions or delegated agreements.
5. Track Every Application and Response
Credentialing isn’t “set it and forget it.”
Use a tracker to log:
- Submission dates
- Assigned payer reps
- Follow-up timelines
- Any required corrections or resubmissions
Check back every 2–3 weeks. Many credentialing stalls happen because someone’s waiting on someone—and no one knows who.
6. Prep Your Billing and UR While You Wait
Yes, you can bill once credentialed—but smart teams prep now.
While credentialing is in progress, get ahead of your operations:
- Enroll with your clearinghouse
- Collect EDI payer IDs
- Train your clinical staff on documentation best practices
- Start utilization review workflows early
This is where Capture’s utilization review services come in—we bridge the gap between credentialing and clean claims.
Real-World Scenario: One Form, One Month, One Fix
A small IOP program in Ohio lost 30 days of billing because one therapist’s NPI number was missing a digit on their CAQH profile. That one typo delayed credentialing with three payers.
The fix took five minutes. The lost revenue? Over $12,000.
Lesson learned: Credentialing isn’t just about red tape. It’s about building the foundation of your entire revenue stream.
Ready to Feel Confident in Your Credentialing Process?
You don’t have to chase paperwork or stress over every portal. Capture RCM helps new providers build strong systems—starting with credentialing and flowing all the way through billing.
Call (380) 383-6822 or visit online to learn more about our utilization review services in the United States. We make utilization review simple—no delays, no red tape, just the trusted support you need to keep care moving forward.