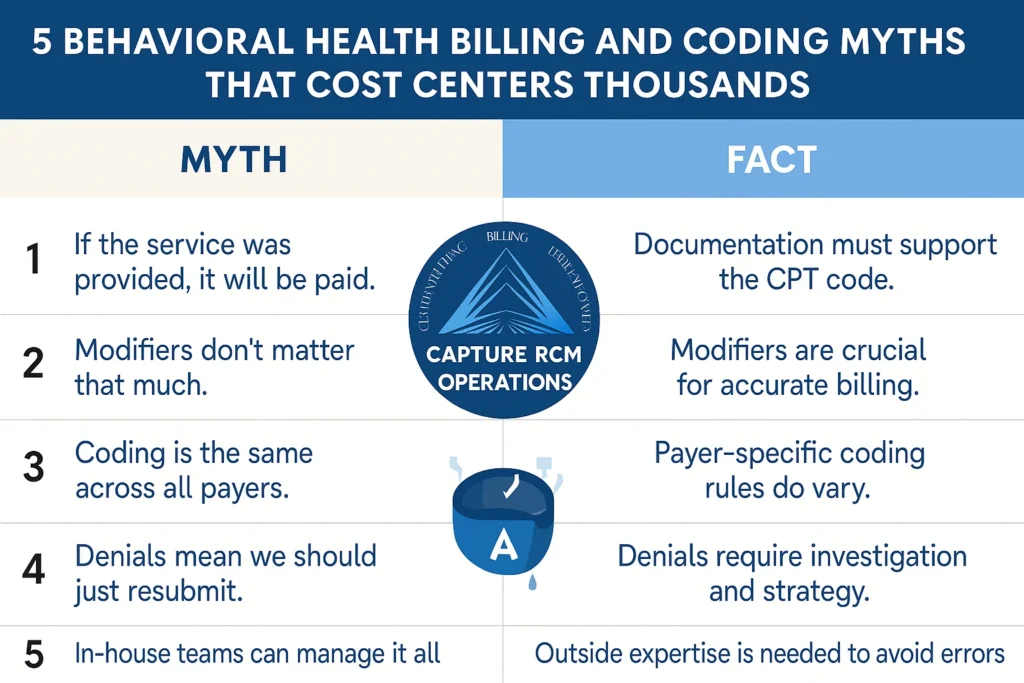
You’ve seen it before—claims denied for reasons that don’t make sense, balances aging out, and revenue slipping away. Often, it’s not the work your team is doing wrong—it’s the myths about billing and coding that keep treatment centers stuck.
The truth? These myths cost centers thousands every month. With the right billing and coding services, you can replace confusion with clarity—and protect your margins.
Myth #1: “If the Service Was Provided, It Will Be Paid”
Reality check: Payers don’t reimburse based on effort—they reimburse based on compliance. If documentation doesn’t fully support the CPT code, reimbursement is at risk. This is why detailed chart audits and coding reviews before submission are essential.
Myth #2: “Modifiers Don’t Matter That Much”
Wrong. Modifiers are not optional—they’re compliance checkpoints. The wrong modifier can trigger denials, audits, or even allegations of fraud. Clean modifier use is one of the most overlooked ways to speed up reimbursement.
Myth #3: “Coding Is the Same Across All Payers”
Nope. What one payer accepts, another may reject. Each payer—and sometimes each state—has its own quirks. Best practice: track payer-specific coding patterns and adapt claims proactively. This is where specialized billing and coding services save hours of rework.
Myth #4: “Denials Mean We Should Just Resubmit”
Simply hitting resubmit is like trying the same key in a locked door. Denials require investigation, root cause analysis, and appeal strategies—not guesswork. Ignoring this step is one of the fastest ways to inflate A/R balances.
👉 Consider pairing billing and coding with utilization review support for stronger medical necessity appeals.
Myth #5: “In-House Teams Can Manage It All”
Even the most experienced in-house billing team can’t realistically keep up with constant payer updates, compliance changes, and coding rules. Without outside expertise, revenue leaks become routine. Partnering with experts prevents A/R from turning into a permanent backlog.
Why Expert Billing and Coding Services Pay Off
At Capture RCM Operations, our billing and coding specialists don’t just process claims—they proactively identify compliance gaps, track payer quirks, and prevent costly mistakes. It’s the difference between hoping for reimbursement and getting paid the first time.
Stop Losing Revenue to Myths
Don’t let billing and coding myths drain your cash flow. Call (380) 383-6822 or visit our billing and coding services page to learn more about how Capture RCM helps behavioral health providers across the United States get paid faster and with confidence.