It doesn’t hit you during the ribbon-cutting or the team meetings. It hits you at 10:42 PM—when you’re alone in the office, staring at another rejected claim and wondering how a thriving caseload still leaves your bank account empty.
If you’re a behavioral health provider who just launched a new treatment program, you’re probably feeling it too: the weight of doing it all. And somewhere between client care, staff support, and endless documentation, revenue cycle management gets treated like an afterthought—until it’s the fire you can’t ignore.
Revenue Isn’t Just a Back-End Problem
Most practice owners think billing is what happens after care is delivered. That’s the first mistake. In reality, revenue cycle management (RCM) starts long before the first session and doesn’t end when a claim is submitted. It’s a full-system process that connects eligibility, authorizations, billing, follow-up, and patient communication.
If you’re only focused on claims, you’re already behind.
You Can’t Fix a System You Haven’t Mapped
Overwhelm often comes from the invisible. If no one ever taught you how to track aging reports, identify code-level denials, or monitor underpayments—it’s not your fault. But it is your responsibility to bring in someone who can.
Successful practice owners don’t know everything about RCM. They just know who to trust.
The Right Billing Partner Doesn’t Just “Do Billing”
A solid RCM partner doesn’t just take claims off your plate—they make your whole practice feel lighter. That means fixing intake workflows, tightening up authorizations, cleaning up credentialing gaps, and building reporting that actually tells you something useful.
At Capture RCM, we help behavioral health practices stop surviving and start scaling—with clarity, not chaos.
Denials Aren’t Just Annoying—They’re Data
Every denial has a story. It’s easy to ignore them or blame the insurer, but behind each one is a pattern: a documentation gap, a code mismatch, a credentialing error. When those stories pile up, they become revenue loss. But when you investigate and resolve them systematically? That’s where growth lives.
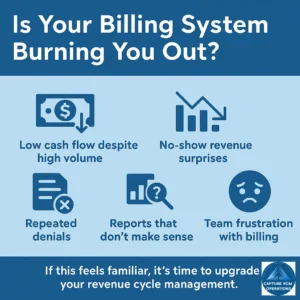
Burnout Often Begins in the Billing Department
You didn’t open a practice to chase down insurance companies. And your team didn’t sign up to spend half their time fixing payment issues instead of supporting clients. Broken RCM processes don’t just bleed money—they bleed morale.
Fix the system, and you free your team to do what they’re actually trained to do.
This Isn’t About Getting Rich—It’s About Staying Open
We’ve seen too many passionate providers burn out or shut down—not because they weren’t good at their work, but because their operations couldn’t sustain their mission. Revenue cycle management is the lifeline. When it’s healthy, everything else gets to breathe.
Real Practices. Real Change.
“I can’t stress enough how much Capture has helped. I used to go to bed dreading the morning—knowing I’d wake up to denials, missing authorizations, and billing fires. Now the system runs smooth, reports make sense, and I finally get to focus on patients instead of paperwork.”
-Outpatient Practice Owner, 2024
📞 Ready to take the weight off your shoulders?
Call (380) 383-6822 or visit us online and see if we can help take the load of billing and credentialing stress off you hands, Services in Ohio, Indiana, Kentucky.


